- Augusta University
- Colleges & Schools
- Medical College of Georgia
- Pediatrics
- Allergy-Immunology Fellowship
- Selner's Rhinolaryngoscopy Online
- Selner's Rhinolaryngoscopy Online
Selner's Rhinolaryngoscopy Online

John C. Selner, MD
William K. Dolen, MD
Bryan Spofford, MD
Jerald W. Koepke, MD
INTRODUCTION
Traditional methods for examination of the nose and throat have limited the extent to which physicians could evaluate symptoms referable to structures of the upper airway. Because the physician often could not actually see the area of complaint, the interpretation of patient symptoms has been limited to the ability of the patient to describe sensation and function. Roentgenographs offer only a static glimpse of the dynamic function of these areas, and the intricate bony structure of the skull makes interpretation of x-rays difficult. Early endoscopists attempted examination of the upper airway with cystoscopes, bronchoscopes, and gastrointestinal endoscopes. Rigid nasal endoscopes were eventually developed, but were difficult to use, uncomfortable for the patient, and were almost exclusively used by otolaryngologists. The medical and industrial development of flexible fiberoptic technology has made a safe, convenient, and inexpensive alternative to previous practice available to any physician interested in comprehensive evaluation of the upper airway. The flexible fiberoptic rhinolaryngoscope places the physician who evaluates and manages patients with upper airway complaints at the same advantage as his pulmonary and gastroenterology colleagues who routinely perform endoscopic examinations.
Aside from specific identification of pathology and the visual surveillance of function, rhinolaryngoscopy offers a unique advantage to the physician interested in assessing the effects of drug therapy and provocation challenges. Bronchial provocation challenges are usually monitored by pulmonary function tests. Rhinomanometry is occasionally used as an objective measure of nasal function, but direct inspection and the recording of symptom scores are more commonly used methods. A quantitative method developed at the Allergy Respiratory Institute of Colorado for evaluation of nasal airway function using a fiberoptic rhinolaryngoscope offers an added dimension in the documentation of specific changes in upper airway physiology induced by medication or provocation challenges.
As is the case with any diagnostic skill, appropriate utilization of the fiberoptic endoscope requires a disciplined commitment to the mastery of the basic science of the upper airway. Although these areas are not emphasized in many medical school curricula, the upper airway has immediate relevance to both the understanding of potential mechanisms operating in host defense and the homeostatic functions of respiration. Humidification, heat regulation, air filtration, and flow dynamics involved in the presentation of air for gas exchange in the lungs are fundamental considerations in the disciplines of otolaryngology, allergy, pulmonary medicine, environmental illness, neurotoxicology, and sleep physiology.
The thought of developing competence in upper airway examination may be intimidating. One need only recall first awkward attempts to drive a car, a medical student's anxiety in examining the tympanic membrane of a struggling 12-month-old, or the difficulty in distinguishing a split S1 from an S4 gallop in order to realize that skill in the performance of fiberoptic rhinolaryngoscopy requires not only a basic understanding of related anatomy, physiology, and pathology but also relatively frequent use of the endoscope, ideally in collaboration with a clinician with experience in the examination of the upper airway.
We believe that nearly any motivated physician can learn to integrate fiberoptic rhinolaryngoscopy into office practice. It is our purpose to make this examination cost and time effective for physicians while accomplishing as complete an examination as possible with minimum discomfort for the patient. These examinations have contributed significantly to the interpretation of patient complaints and have influenced therapeutic decision-making. We suggest that rhinolaryngoscopy should be taught early in the course of training in allergy or otolaryngology, where the procedure can be used as a means of teaching upper airway anatomy and pathology as well as a way to facilitate collaboration, rather than competition, with other specialists. Intelligent use of fiberoptic rhinolaryngoscopy will result in early and appropriate requests for consultation. We emphatically do not believe that fiberoptic rhinolaryngoscopy, when used as an adjunct to routine upper airway examination, should contribute substantial cost to a medical evaluation.
This workbook is a compilation of the lectures, handouts, and videotaped material used to introduce more than a thousand physicians to this procedure at national medical meetings and at courses taught in a medical office. At their request, we have developed it both to share our practical experience in fiberoptic endoscopy of the upper airway and to provide physicians with a concise and pragmatic text of upper airway anatomy and pathology.
ACKNOWLEDGEMENTS
We wish to thank Ray Wood, M.D., Department of Otorhinolaryngology, University of Colorado Health Sciences Center, for his help in development of the methods described in this workbook. Kent Christopher, M.D., a chest physician from the Institute for Transtracheal Oxygen Therapy at Presbyterian/St. Luke's Medical Center, Denver, provided critical guidance and encouragement. Gail Glover's attention to detail in the documentation and cataloging of photographic material was invaluable. Toni Pawlowsky made the original anatomic drawings from which computer graphics were later generated. This second edition of the workbook was produced using a desktop publishing system consisting of a Macintosh Plus computer and LaserWriter printer using MacWrite 5.0, Pagemaker 3.0, and Illustrator 88 software.
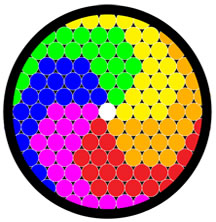
It has been 20 years since the publication of the second edition of Rhinolaryngoscopy. Back then, it would have been nice to have color illustrations and images included in the body of the text, but the cost was prohibitive. We thought it would be better to include 35mm slides that could be used in lectures. Web technology now makes it possible to make Selner's Rhinolaryngoscopy available to a new generation of allergists in an improved format.
In memoriam, John Canty Selner, MD (1936-2006)