
- Augusta University
- Colleges & Schools
- Medical College of Georgia
- Physiology
- Research Opportunities for Clinicians
Research Opportunities for Clinicians
These faculty members are offering to be mentors to Residents looking for an opportunity to acquire hands-on experience in research as part of their training.
This one year program is full time in a research lab with the expectation that the Resident will present at national/international meetings, compete for research awards, and publish one or more papers.
Cardiovascular
Zsolt Bagi, MD, PhD - Professor - Physiology
706-721-3423 / zbagi@augusta.edu / Grant Support: R01, AHA / CV
Our studies in the Bagi Lab focus on the investigation of the function of small blood vessels. We want to develop a greater understanding of how coronary resistance arteries are controlled in health and disease, and how dysfunction of arteries contribute to organ failure. Our goal is to discover new vascular targets for therapeutic intervention of coronary heart disease and heart failure.

Michael Brands, PhD - Regents' Professor - Physiology
706-721-9785 / mbrands@augusta.edu / Grant Support: P01 Program Director, R01 / CV
Cardiovascular-renal integrative physiology and hypertension. Longstanding interest in renal and hormonal mechanisms for chronic blood pressure and circulatory system control in states of insulin resistance, hyperinsulinemia, and diabetes.
Yanbin Dong, MD, PhD - Regents' Professor - Georgia Prevention Institute Department of Medicine
706-721-9785 / ydong@augusta.edu / Grant Support: Two R01s / CV
My research areas include clinical trials, pharmacological intervention, nutritional supplementation, genetics/epigenetics, biomarkers and inflammation underlying obesity, hypertension, and cardiovascular disease.
Jessica Filosa, PhD - Professor - Physiology
706-721-8901 / jfilosa@augusta.edu / Grant Support: Two R01s / CV
My major research interest is to gain understanding of the signaling mechanisms governing bi-directional communication among the various cell types within the brain. In particularly, I am interested in the communication between neurons and their surrounding glial and vascular cells. Recent findings have demonstrated an important role for astrocytes as intercellular bridges between the state of neuronal activity and vascular dynamics (or neurovascular coupling). These findings have led to a number of different hypotheses addressing the potential role astrocytes have in neurovascular coupling.

Ryan Harris, PhD - Professor - Department of Medicine
706-721-5998 / ryharris@augusta.edu / Grant Support: Clinical Research Grant, Two R01s, Vertex Pharmaceuticals IIS Grant, AHA SFRN / CV
Cardiovascular disease remains the number one cause of death in the United States. Under the direction of Dr. Ryan A. Harris, PhD, CEP, FACSM, the mission of the Laboratory of Integrative Vascular and Exercise Physiology (LIVEP) is to conduct cutting-edge research that integrates vascular and exercise physiology to understand how blood vessels contribute to disease development. Visit us on the web at www.livep.net to learn more about what we do.
David Mattson, PhD - Department Chair and Professor
706-721-7742 / dmattson@augusta.edu / Grant Support: P01 Project, R01 / CV
Studies in the Mattson laboratory examine the normal and pathophysiological regulation of renal function and arterial blood pressure. A particular emphasis is placed on the paracrine, autocrine, and hormonal regulation of renal tubular and vascular function. Additional studies are geared toward an understanding of the genetic basis of hypertension and renal disease.
Paul O'Connor, PhD - Professor - Physiology
706-721-7890 / paoconnor@augusta.edu / Grant Support: Project Leader P01, R21 / CV
Our laboratory’s primary research interests lie in the physiological pathways involved in the regulation of kidney function and how disruptions in these pathways can lead to disease. Recently our laboratory has also become interested in the mechanisms through which splenic anti-inflammatory pathways regulate the innate immune response.

R. Daniel Rudic, PhD - Associate Professor - Pharmacology and Toxicology
706-721-7649 / rrudic@augusta.edu / Grant Support: NIA R01 and supplement / CV
My research laboratory is interested in understanding how the molecular mechanisms that control circadian rhythms (circadian clocks) act on the cardiovascular system to influence artery function and disease. We are particularly interested in defining the particular role of endothelial cells that make up the blood vessel, and we are now endeavoring on some new ground for us in neuroscience with the support of the National Institute of Aging. We are seeking to determine how and if we can observe interactions between blood vessel disease, clocks, and the brain during aging and Alzheimer's disease using mouse models.
Dr. Rudic's Publications

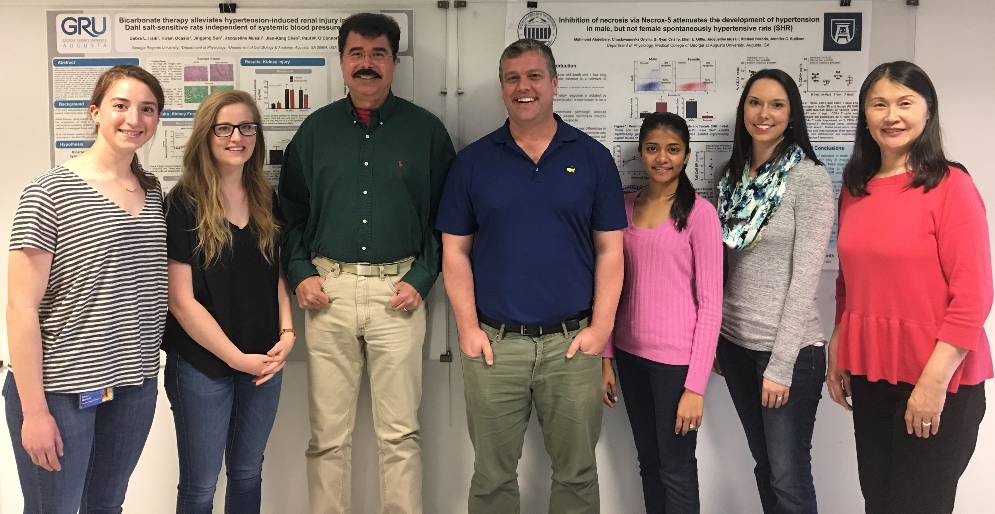
Jennifer Sullivan, PhD - Professor - Physiology
706-721-9796 / jensullivan@augusta.edu / Grant Support: AHA Grant In Aid, Project Leader P01, R01 / CV
The overall goal of my laboratory is to better understand the molecular mechanisms that regulate blood pressure in males and females under both physiological and pathophysiological conditions, including hypertension. Traditionally, it has been assumed that blood pressure control and the basis of hypertension is the same in males and females; just the magnitude of the response differs. However, based on the vast number of differences that have been identified in cardiovascular physiology, pathophysiology, and pharmacology between the sexes, there is growing evidence to suggest that the pathways by which males and females develop cardiovascular and renal diseases may be distinct. Ongoing studies are focused on 3 pathways involved in blood pressure control and cardiovascular function: the renin angiotensin system (RAS), the nitric oxide (NO) pathway, and inflammation.
Mong-Heng Wang, PhD - Associate Professor - Physiology
706-721-3830 / mwang@augusta.edu / Grant Support: AHA Grant In Aid / CV
I have worked in the field of cytochrome P450 (CYP)-derived eicosanoids in cardiovascular diseases, renal diseases, and diabetes for more than 20 years. Throughout these years we have identified new compounds and pathways and elucidated their biological activities and their therapeutically potential for treatment of cardiovascular and diabetes-associated disorders.
Diabetes

Michael Brands, PhD - Regents' Professor - Physiology
706-721-9785 / mbrands@augusta.edu / Grant Support: P01 Program Director, R01 / CV
Cardiovascular-renal integrative physiology and hypertension. Longstanding interest in renal and hormonal mechanisms for chronic blood pressure and circulatory system control in states of insulin resistance, hyperinsulinemia, and diabetes.
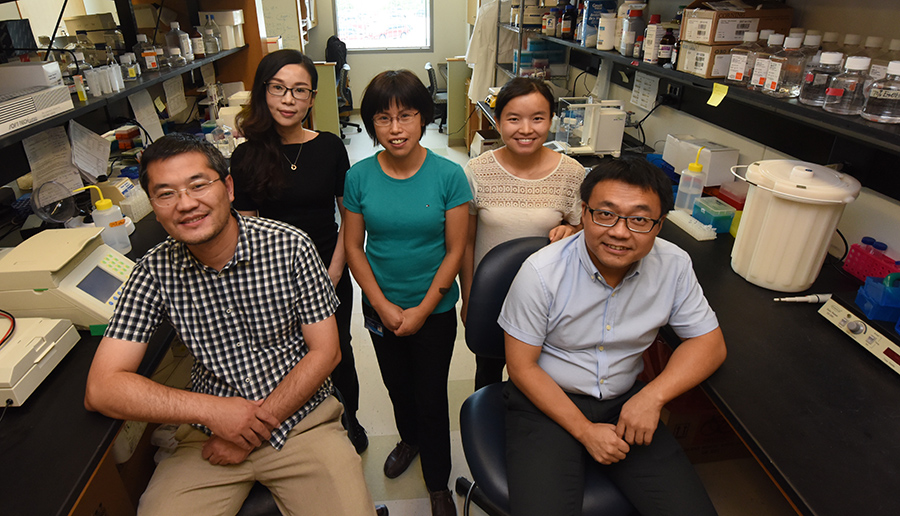
Weiqin Chen, PhD - Associate Professor - Physiology
706-721-8706 / wechen@augusta.edu / Grant Support: R01 / CV
Obesity and its associated health comorbidities are a worldwide epidemic with serious economic and health burden on society. The long-term research interest in the lab is to understand the regulation of white, beige and brown adipose tissue development and energy homeostasis, and use it to develop potential therapeutic approaches for obesity and related metabolic diseases.

Ryan Harris, PhD - Professor - Department of Medicine
706-721-5998 / ryharris@augusta.edu / Grant Support: Clinical Research Grant, Two R01s, Vertex Pharmaceuticals IIS Grant, AHA SFRN / CV
Cardiovascular disease remains the number one cause of death in the United States. Under the direction of Dr. Ryan A. Harris, PhD, CEP, FACSM, the mission of the Laboratory of Integrative Vascular and Exercise Physiology (LIVEP) is to conduct cutting-edge research that integrates vascular and exercise physiology to understand how blood vessels contribute to disease development. Visit us on the web at www.livep.net to learn more about what we do.
Mong-Heng Wang, PhD - Associate Professor - Physiology
706-721-3830 / mwang@augusta.edu / Grant Support: AHA Grant In Aid / CV
I have worked in the field of cytochrome P450 (CYP)-derived eicosanoids in cardiovascular diseases, renal diseases, and diabetes for more than 20 years. Throughout these years we have identified new compounds and pathways and elucidated their biological activities and their therapeutically potential for treatment of cardiovascular and diabetes-associated disorders.
Hormones

Wendy Bollag, PhD - Professor - Physiology
706-721-0698 / wbollag@augusta.edu / Grant Support: VA Merit Award, R01, T35 / CV
My research interests lie in understanding the mechanisms by which hormones, growth factors, cytokines and other signaling molecules instruct cells to respond appropriately to perform their functions. Our current project is investigating the regulation of keratinocyte growth and differentiation and a second defining the signaling mechanisms regulating aldosterone secretion from the adrenal gland. In the first project in skin, we are defining the role of the signaling enzymes phospholipase D (PLD) in promoting epidermal keratinocyte differentiation and protein kinase D (PKD) in supporting keratinocyte proliferation and survival.

Michael Brands, PhD - Regents' Professor - Physiology
706-721-9785 / mbrands@augusta.edu / Grant Support: P01 Program Director, R01 / CV
Cardiovascular-renal integrative physiology and hypertension. Longstanding interest in renal and hormonal mechanisms for chronic blood pressure and circulatory system control in states of insulin resistance, hyperinsulinemia, and diabetes.

Ruth Harris, PhD - Regents' Professor - Physiology
706-721-4479 / ruharris@augusta.edu / Grant Support: Two R01s / CV
My research focuses on factors that influence the control of food intake, body weight and body composition. We have an emphasis on the role of leptin, a hormone that is secreted by adipose tissue and acts to suppress food intake as well as modify peripheral metabolism and insulin sensitivity. Currently, we are examining how leptin responses in different areas of the brain are integrated to reduce meal size, energy intake and body fat mass.

David Mattson, PhD - Department Chair and Professor - Physiology
706-721-7742 / dmattson@augusta.edu / Grant Support: P01 Project, R01 / CV
Studies in the Mattson laboratory examine the normal and pathophysiological regulation of renal function and arterial blood pressure. A particular emphasis is placed on the paracrine, autocrine, and hormonal regulation of renal tubular and vascular function. Additional studies are geared toward an understanding of the genetic basis of hypertension and renal disease.

Jennifer Sullivan, PhD - Professor - Physiology
706-721-9796 / jensullivan@augusta.edu / Grant Support: AHA Grant In Aid, Project Leader P01 / CV
The overall goal of my laboratory is to better understand the molecular mechanisms that regulate blood pressure in males and females under both physiological and pathophysiological conditions, including hypertension. Traditionally, it has been assumed that blood pressure control and the basis of hypertension is the same in males and females; just the magnitude of the response differs. However, based on the vast number of differences that have been identified in cardiovascular physiology, pathophysiology, and pharmacology between the sexes, there is growing evidence to suggest that the pathways by which males and females develop cardiovascular and renal diseases may be distinct. Ongoing studies are focused on 3 pathways involved in blood pressure control and cardiovascular function: the renin angiotensin system (RAS), the nitric oxide (NO) pathway, and inflammation.

“The measure of greatness in a scientific idea is the extent to which it stimulates thought and opens up new lines of research.”
Paul Dirac
Kidney

Michael Brands, PhD - Regents' Professor - Physiology
706-721-9785 / mbrands@augusta.edu / Grant Support: P01 Program Director, R01 / CV
Cardiovascular-renal integrative physiology and hypertension. Longstanding interest in renal and hormonal mechanisms for chronic blood pressure and circulatory system control in states of insulin resistance, hyperinsulinemia, and diabetes.

Mykola Mamenko, PhD - Assistant Professor - Physiology
706-721-9103 / mmamenko@augusta.edu / CV
Our research is focused on the cellular and molecular mechanisms governing water and electrolyte handling in the kidney. The laboratory pursues a few lines of inquiry: we study how disrupted calcium homeostasis in renal epithelial cells is associated with polycystic kidney disease (PKD) and nephrogenic diabetes insipidus (NDI), investigate sex-specific mechanisms governing final regulation of sodium reabsorption in the kidney, critical for the chronic blood pressure control.

David Mattson, PhD - Department Chair and Professor - Physiology
706-721-7742 / dmattson@augusta.edu / Grant Support: P01 Project, R01 / CV
Studies in the Mattson laboratory examine the normal and pathophysiological regulation of renal function and arterial blood pressure. A particular emphasis is placed on the paracrine, autocrine, and hormonal regulation of renal tubular and vascular function. Additional studies are geared toward an understanding of the genetic basis of hypertension and renal disease.
Paul O'Connor, PhD - Professor - Physiology
706-721-7890 / paoconnor@augusta.edu / Grant Support: Project Leader P01, R21 / CV
Our laboratory’s primary research interests lie in the physiological pathways involved in the regulation of kidney function and how disruptions in these pathways can lead to disease. Recently our laboratory has also become interested in the mechanisms through which splenic anti-inflammatory pathways regulate the innate immune response.

Jennifer Sullivan, PhD - Professor - Physiology
706-721-9796 / jensullivan@augusta.edu / Grant Support: AHA Grant In Aid, Project Leader P01 / CV
The overall goal of my laboratory is to better understand the molecular mechanisms that regulate blood pressure in males and females under both physiological and pathophysiological conditions, including hypertension. Traditionally, it has been assumed that blood pressure control and the basis of hypertension is the same in males and females; just the magnitude of the response differs. However, based on the vast number of differences that have been identified in cardiovascular physiology, pathophysiology, and pharmacology between the sexes, there is growing evidence to suggest that the pathways by which males and females develop cardiovascular and renal diseases may be distinct. Ongoing studies are focused on 3 pathways involved in blood pressure control and cardiovascular function: the renin angiotensin system (RAS), the nitric oxide (NO) pathway, and inflammation.

"SOMEWHERE, SOMETHING INCREDIBLE IS WAITING TO BE KNOWN."
Carl Sagan
Neuroscience
Jessica Filosa, PhD - Professor - Physiology
706-721-8901 / jfilosa@augusta.edu / Grant Support: Two R01s / CV
My major research interest is to gain understanding of the signaling mechanisms governing bi-directional communication among the various cell types within the brain. In particularly, I am interested in the communication between neurons and their surrounding glial and vascular cells. Recent findings have demonstrated an important role for astrocytes as intercellular bridges between the state of neuronal activity and vascular dynamics (or neurovascular coupling). These findings have led to a number of different hypotheses addressing the potential role astrocytes have in neurovascular coupling.

Philip O'Herron, PhD - Research Assistant Professor - Physiology
706-721-9103 / poherron@augusta.edu / Grant Support: R21 / CV
My lab’s research focuses on questions of neurovascular coupling and visual processing. Our neurovascular coupling works seeks to determine how neural activity in the cortex drives the hemodynamic responses (functional hyperemia) and, in turn, how neurons depend on the increased blood flow to active regions.

Ruth Harris, PhD - Regents' Professor - Physiology
706-721-4479 / ruharris@augusta.edu / Grant Support: Two R01s / CV
My research focuses on factors that influence the control of food intake, body weight and body composition. We have an emphasis on the role of leptin, a hormone that is secreted by adipose tissue and acts to suppress food intake as well as modify peripheral metabolism and insulin sensitivity. Currently, we are examining how leptin responses in different areas of the brain are integrated to reduce meal size, energy intake and body fat mass.
Obesity
Yanbin Dong, MD, PhD - Regents' Professor - Georgia Prevention Institute Department of Medicine
706-721-9785 / ydong@augusta.edu / Grant Support: Two R01s / CV
My research areas include clinical trials, pharmacological intervention, nutritional supplementation, genetics/epigenetics, biomarkers and inflammation underlying obesity, hypertension, and cardiovascular disease.
Weiqin Chen, PhD - Associate Professor - Physiology
706-721-8706 / wechen@augusta.edu / Grant Support: R01 / CV
Obesity and its associated health comorbidities are a worldwide epidemic with serious economic and health burden on society. The long-term research interest in the lab is to understand the regulation of white, beige and brown adipose tissue development and energy homeostasis, and use it to develop potential therapeutic approaches for obesity and related metabolic diseases.

Ruth Harris, PhD - Regents' Professor - Physiology
706-721-4479 / ruharris@augusta.edu / Grant Support: Two R01s / CV
My research focuses on factors that influence the control of food intake, body weight and body composition. We have an emphasis on the role of leptin, a hormone that is secreted by adipose tissue and acts to suppress food intake as well as modify peripheral metabolism and insulin sensitivity. Currently, we are examining how leptin responses in different areas of the brain are integrated to reduce meal size, energy intake and body fat mass.

"To raise new questions, new possibilities, to regard old problems from a new angle, requires creative imagination and marks real advance in science."
Albert Einstein
Skin

Wendy Bollag, PhD - Professor - Physiology
706-721-0698 / wbollag@augusta.edu / Grant Support: VA Merit Award, R01, T35 / CV
My research interests lie in understanding the mechanisms by which hormones, growth factors, cytokines and other signaling molecules instruct cells to respond appropriately to perform their functions. Our current project is investigating the regulation of keratinocyte growth and differentiation and a second defining the signaling mechanisms regulating aldosterone secretion from the adrenal gland. In the first project in skin, we are defining the role of the signaling enzymes phospholipase D (PLD) in promoting epidermal keratinocyte differentiation and protein kinase D (PKD) in supporting keratinocyte proliferation and survival.

"Scientific research is one of the most exciting and rewarding of occupations."
Frederick Sanger