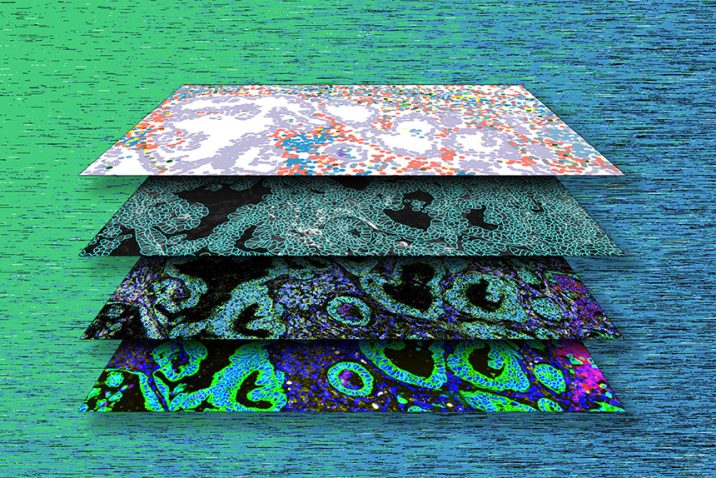
Medical College of Georgia partners in $3.3 million NIH grant studying antibiotic resistance
An Augusta University researcher is partnering with the University of California San Diego to unravel the complexities of Staphylococcus aureus vaccine failures.